Honeybee venom kills aggressive breast cancer cells: Australian study
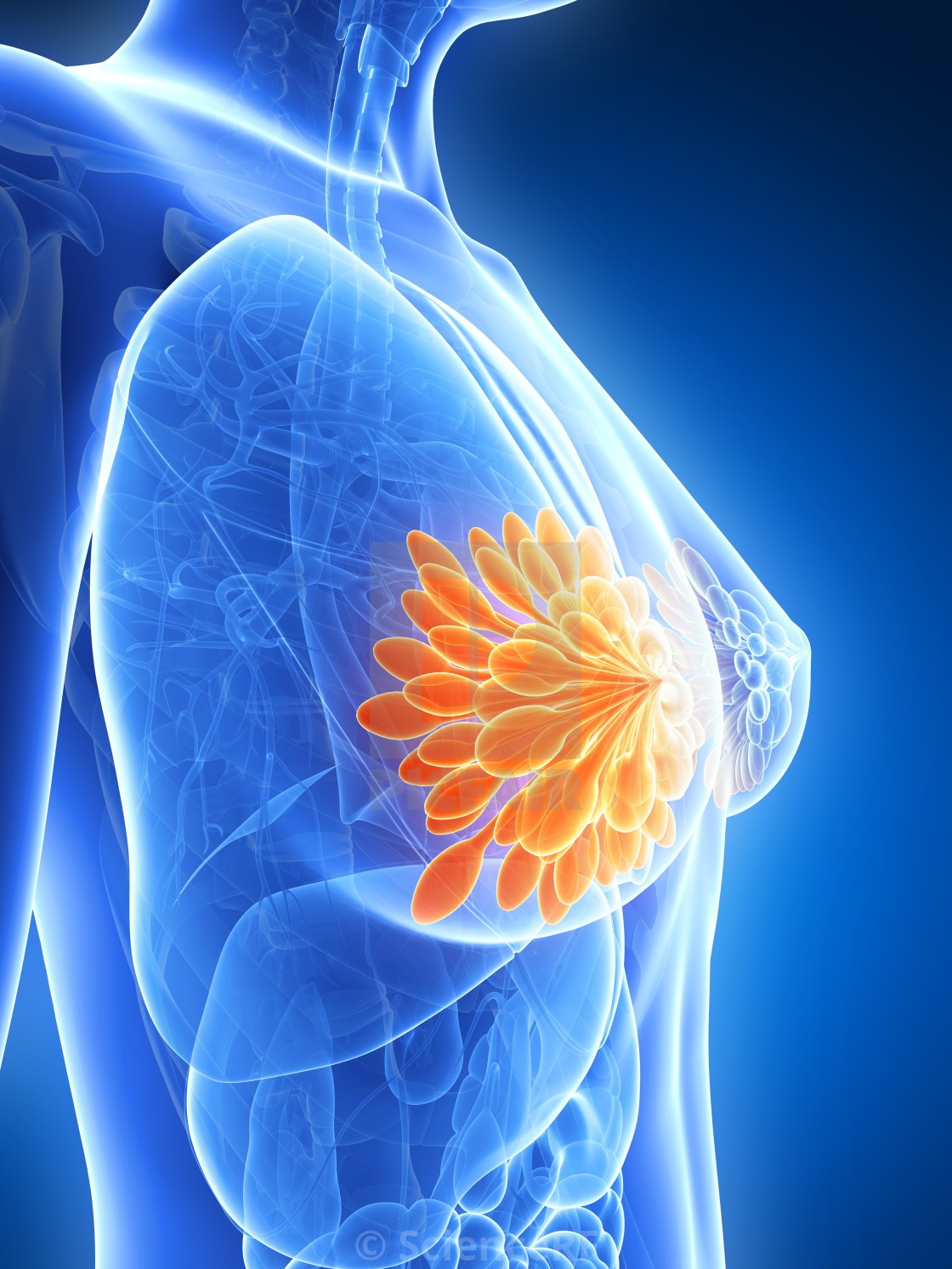
Venom from honeybees has been found to rapidly destroy triple-negative breast cancer and HER2-enriched breast cancer cells – with minimal effect on healthy cells, according to a study published this month.
The study looked at the effect of the European honeybee (Apis mellifera) venom on normal breast cells; and cells from clinical subtypes of breast cancer: hormone receptor positive, HER2-enriched, and triple-negative breast cancer.
The researchers tested melittin – a small, positively charged peptide which is a major component in honeybee venom – as well as a synthetically reproduced version. They found that the synthetic product mirrored the majority of anti-cancer effects of honeybee venom.
Melittin can also be used with small molecules or chemotherapies, such as docetaxel, according to the researchers, who say the combination of melittin and docetaxel was ‘extremely efficient’ in reducing tumor growth in mice.
The findings are important as triple-negative breast cancer and HER2-enriched tumors are highly aggressive breast cancer subtypes. Triple-negative breast cancer in particular is associated with the poorest outcomes and currently has limited treatment options.
Specific concentration of honeybee venom induces 100% cancer cell death
Researchers from the Harry Perkins Institute of Medical Research (Australia) and The University of Western Australia used the venom from 312 Australian, Irish and English honeybees in their study.
As the active component of honeybee venom, melittin is a positively charged, amphipathic 26-amino-acid peptide. Researchers found it was able to target cancer cells by shutting down the activity of molecules overexpressed in these cancers.
“We found both honeybee venom and melittin significantly, selectively and rapidly reduced the viability of triple-negative breast cancer and HER2-enriched breast cancer cells,” said Dr Ciara Duffy. “The venom was extremely potent.”
A specific concentration of honeybee venom can induce 100% cancer cell death, with minimal effects on normal cells, according to the study. Melittin could completely destroy cancer cell membranes within 60 minutes.
Attaching an RGD peptide to melittin (RGD1-melittin) was found to further enhance the targeting of melittin to malignant cells, again with minimal toxicity to normal cells.
Signalling pathways
Melittin was also able to ‘substantially reduce’ the chemical messages needed for cancer cell growth and cell division.
"We looked at how honeybee venom and melittin affect the cancer signalling pathways, the chemical messages that are fundamental for cancer cell growth and reproduction, and we found that very quickly these signalling pathways were shut down,” said Duffy.
"Melittin modulated the signalling in breast cancer cells by suppressing the activation of the receptor that is commonly overexpressed in triple-negative breast cancer, the epidermal growth factor receptor, and it suppressed the activation of HER2 which is over-expressed in HER2-enriched breast cancer.”
Use with small molecule drugs
The researchers also looked at whether melittin could be used with existing chemotherapy drugs, as it forms pores in breast cancer cell membranes, potentially enabling the entry of other treatments into the cancer cell.
"We found that melittin can be used with small molecules or chemotherapies, such as docetaxel, to treat highly-aggressive types of breast cancer,” said Duffy. “The combination of melittin and docetaxel was extremely efficient in reducing tumour growth in mice."
This highlights the potential for melittin for use in combination therapies to potentially increase the efficacy – or reduce the dose – of cytotoxic agents. This in turn would enable more cost-effective treatments, potentially with fewer side effects.
Further studies will be required to formally assess the optimum method of delivery of melittin, as well as toxicities and maximum tolerated doses, say the researchers.
Bee venom
There are around 20,000 species of bees: with the study looking at the European honeybee found in Australia, Ireland and England. The bee populations from each country produced almost identical effects in breast cancer cells.
It also looked at the venom from bumblebees: but this did not have the same effect and was unable to induce cell death.
One of the first reports of the effects of bee venom was published in 1950, where venom reduced the growth of tumours in plants. Over the past two decades, interest in apitherapy has grown, as has interest in the effects on honeybee venom on different cancers.
Despite this, the molecular mechanisms and selectivity of biomolecular components of honeybee venom as anticancer agents remain largely unknown – prompting the new study.
“Understanding the molecular basis and specificity of bee venom against cancer cells is key for developing and optimizing novel effective therapeutics from a natural product that is widely available and cost-effective to produce in many communities around the world,” say researchers.
Wider potential
“Honeybee venom is available globally and offers cost-effective and easily accessible treatment options in remote or less-developed regions,” continue the researchers.
“Further research will be required to assess whether the venom of some genotypes of bees has more potent or specific anticancer activities, which could then be exploited.”
“Beyond breast cancer, tumors overexpressing EGFR include lung, glioblastoma, and colorectal cancers, and tumors that can overexpress HER2 include gastric, ovarian, endometrial, bladder, lung, colon, and head and neck cancers.”
Earlier this year, City of Hope scientists published research on the use of chlorotoxin (CLTX), a component of scorpion venom, with brain tumor cells. The researchers developed and tested the first chimeric antigen receptor (CAR) T cell therapy using chlorotoxin to direct T cells to target brain tumor cells.
Source: npj Precision Oncology, 24 (2020)
Duffy, C., Sorolla, A., Wang, E. et al. Honeybee venom and melittin suppress growth factor receptor activation in HER2-enriched and triple-negative breast cancer. npj Precis. Onc. 4, 24 (2020).
https://doi.org/10.1038/s41698-020-00129-0